TBI Fundamentals
A New Approach to TBI

Dr. Mark Gordon, Millennium Health, Founder and Medical Director
Dr. Gordon has completed extensive research in the area of TBI and PTSD through which he has developed a successful treatment protocol that has been used with thousands of veterans and civilians alike.
Asymmetric Health is a proud member of the Millennium TBI Network and certified in Dr. Gordon’s protocols for treatment of TBI.
TBI Protocol
The Millennium Network TBI protocol utilizes advance diagnostic laboratory testing to assess central and peripheral hormonal deficiencies that can result from TBI. Using a combination of supplements and prescription medications individualized to your specific symptoms and laboratory findings, the TBI protocol seeks to address the underlying neuroinflammatory environment that perpetuates hormonal dysfunction and treats the underlying cause of many of the symptoms experienced by those with TBI. By switching the treatment approach away from symptom management towards an integrative model addressing root cause dysfunction we are able to work on finally getting you back to reclaiming your life.
What is traumatic brain injury?
Traumatic brain injury (TBI) occurs when sudden, physical injury occurs to the brain. Typically, the injuries considered for TBI were the result of external mechanical forces such as closed head injury and penetrating brain trauma.
A closed head injury occurs when there is nonpenetrating external injury to the brain that does not fracture the skull. This type of injury commonly occurs from directly striking the head, rapid acceleration/deceleration, or blast wave trauma. Common causes of this type of injury are auto accidents, falls, assaults, and athletics. For a generation of soldiers, blast wave trauma from improvised explosive devices, repetitive close quarter gun fire, and mortar attack is the hallmark injury from combat operations in Iraq and Afghanistan.
Penetrating brain injury occurs when there is a fracture, or break, in the skull. Think of a gunshot wound or shrapnel injury.
While external injury is classically required for TBI, newer research is beginning to recognize the similarity in injury caused by non-external forces such as critical illness, low oxygen levels, severe hypoglycemia, massive hemorrhage, and stroke.
What is the prevalence of TBI?
In 2010, the CDC estimated that TBIs accounts for approximately 2.5 million emergency department visits, hospitalizations, and deaths in the United States. Since 2000, the DoD has reported 440,000 cases of TBI in service members. These data extraordinarily underestimate the true prevalence of TBI since it does not account for those persons who did not receive medical care, had outpatient or office-based visits, or received care at a federal facility.
Although data are limited, estimates based off of population studies in two US states indicate that there are 3.2 million – 5.3 million persons in the United States living with a TBI-related disability. These numbers do not account for the millions more that are living with chronic non-debilitating sequalae of their injury.
What is the severity of TBI?
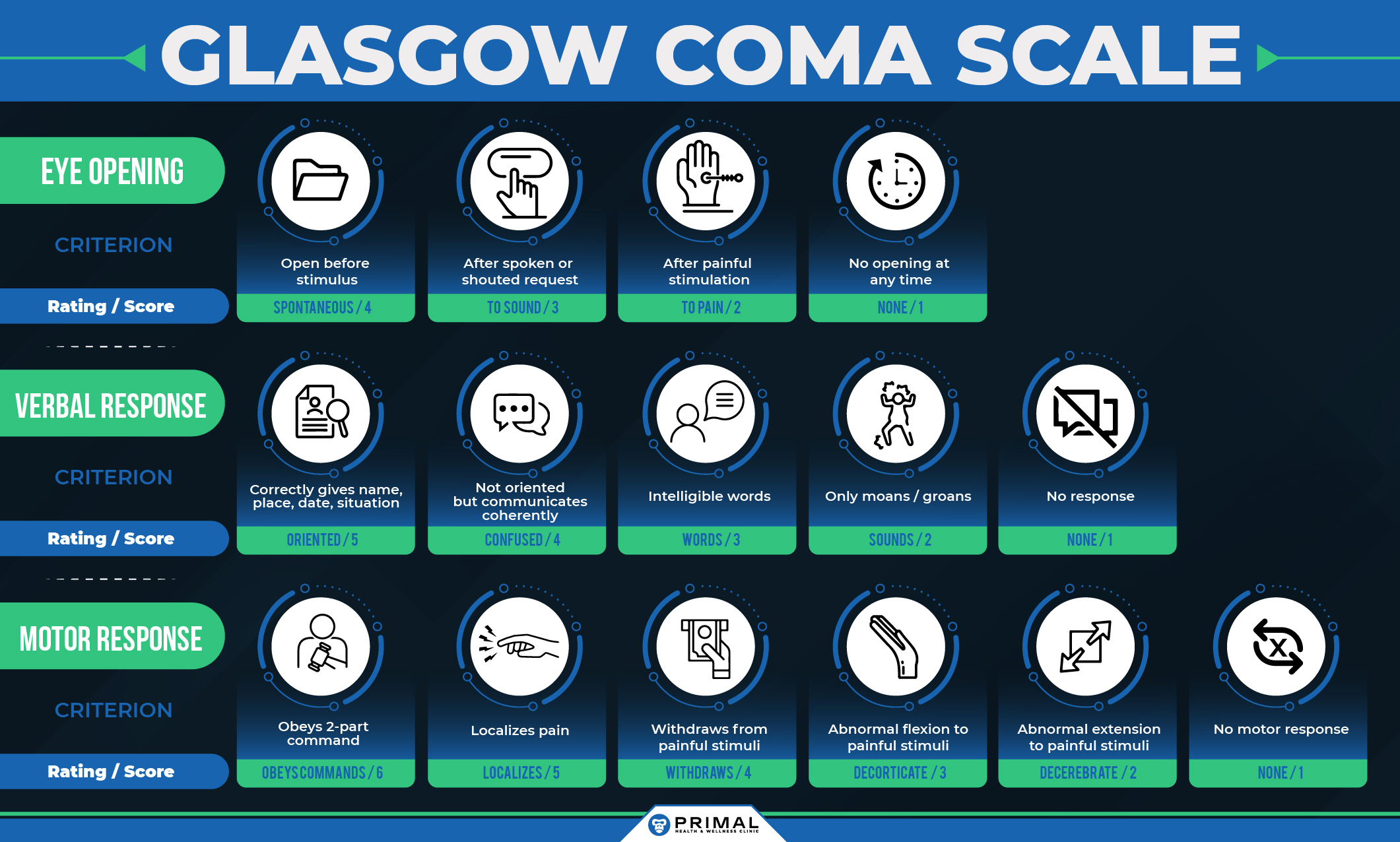
TBI is classified as mild, moderate, or severe depending on the clinical presentation of a patient’s neurological signs and symptoms. There are several classification scales that are used to help rate the severity of TBI including posttraumatic amnesia, loss of consciousness duration, disability rating scale, functional assessment measure, and Rancho Los Amigos scale to name a few. The most commonly used grading system is the Glasgow Coma Scale (GCS).
The GCS is a fifteen-point scale which measures patient’s eye, verbal, and motor responses to various stimuli. A score of 13-15 is considered a mild injury while 8-13 is moderate and below 8 is severe. A mild TBI (mTBI) is synonymous with a concussion. An overwhelming majority of TBIs are mild and estimates are that 66% of those are never evaluated in the medical system. For those who end up developing subtle neuropsychological symptoms long after the initial injury the association between mTBI and the symptoms is frequently lost
What causes the symptoms of TBI?
The degree of symptom development and recovery depends both on the severity of mechanical injury and the underling health of the brain the injury occurs to. The first phase of injury results from the primary mechanical event. The physical forces exerted on the brain inside of the rigid skull can lead to shearing forces, contusion, hemorrhage, edema, ischemia, axonal injury, and blood brain barrier disruption. The resulting damage from the initial phase of injury then sets off a secondary phase of biochemical-inflammatory cascades which create a non-neuropermissive environment (NPE) leading to expanded areas of cellular disruption, neuronal damage, and cavitation.
If an injury is severe enough that a patient seeks medical care, then the initial diagnostic tool used is typically a non-contrast CT scan of the brain. This is an excellent imaging study to rapidly assess for skull fractures and bleeding in the brain (hemorrhage). In severe cases requiring hospitalization MRI is typically used as a secondary imaging modality with greater sensitivity to contusion, swelling, and bleeding. However, even in a vast majority of TBI cases that seek acute medical care the imaging is unremarkable and there are currently no easily performed laboratory tests that allow health care providers to adequately risk stratify patients for severity of ongoing secondary phase injury.
The secondary phase of injury occurs in the immediate aftermath of the initial mechanical force. There are six major simultaneous, intertwined cascades of damage that occur during this phase.
- Inflammation
- Excitotoxicity
- Mitochondrial Dysfunction
- Oxidative stress
- Blood brain barrier disruption
- Cell death
Increased stimulation of ionotropic glutamate receptors (NMDA, AMPAR, and KA) leads to increased sodium entry into the neurons contributing to membrane depolarization and swelling. This also leads to increases calcium entry into the cell which can trigger downstream disruption of mitochondrial energy synthesis, excitatory neurotransmitter release, and overstimulation of inflammatory enzymes.
Mitochondria are the energy production factories of your cells. When your brain tissue is injured there is increased energy demand placed on the mitochondrial to facilitate repair. However, when the energy requirement exceeds the mitochondria’s collective ability for adequate energy production there is increased generation of mitochondrial reactive oxygen species (ROS) which can quickly overwhelm your natural antioxidant defense system. The accumulation of ROS further exacerbates mitochondrial respiratory dysfunction leading to mitochondrial degradation, excitotoxicity and apoptotic cellular signaling.
Your central nervous system (brain and spinal cord) is separated from your systemic blood circulation by the blood-brain barrier (BBB). The BBB protects your CNS from blood-borne compounds such as toxins, chemicals, antibodies, antigens, bacteria, and viruses. Strict homeostasis of the BBB is required for optimal functioning of your CNS. In TBI, local and peripheral production of inflammatory signalers can lead to the loss of integrity of the tight junctions between cells that make up the BBB. Once selective permeability of the BBB is disrupted peripherally circulating compounds can gain access to the CNS leading to further cellular disruption to damaged brain tissue.
There are several different types of cell death and damage; necrosis, apoptosis, parthanatos, and autophagy. Necrosis is the uncontrolled destruction of the cell. This process not only results in the death of the cell but also leads to the release of numerous free radicals and signaling molecules that damage surrounding cells. Apoptosis and parthanatos are cellular death mechanisms that are more controlled than necrosis. If necrosis is cellular murder, then apoptosis and parthantos are cellular suicide. Both are mechanisms of cell death but cause less damage to surrounding cells than necrosis. Autophagy is when a cell is able to survive by quarantining off damaged cytoplasmic material for controlled destruction. Only parts of the cell are destroyed but the entire cell is able to survive and regenerate damaged organelles. The combination of inflammation, excitotoxicity, mitochondrial disruption, oxidative stress, and BBB disruption determine the amount and type of cell death that occurs during the second phase of injury from TBI.
What are the symptoms of TBI?
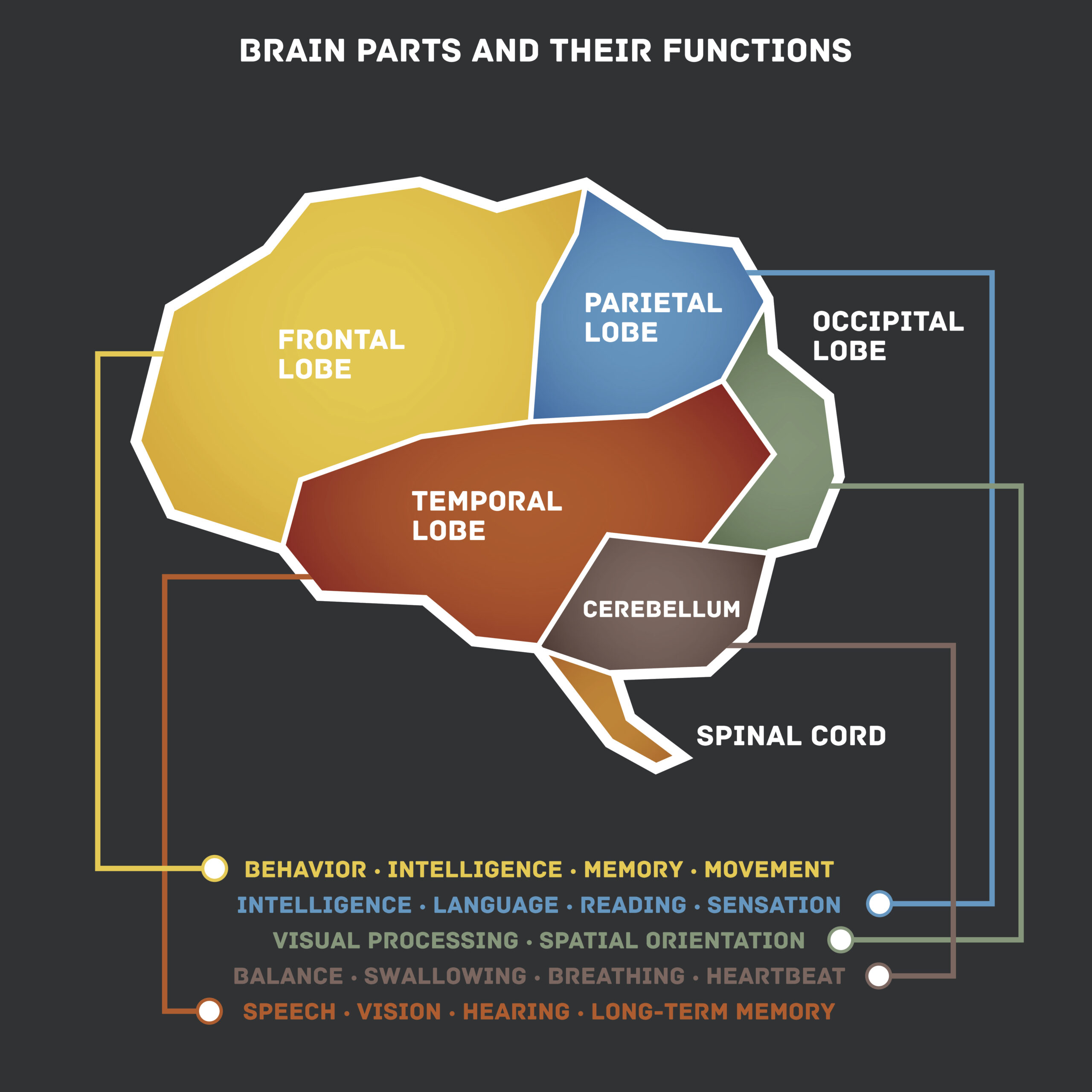
The symptoms of TBI are as varied as the brains it occurs to. Generally speaking, symptoms can be grouped into broad domains (physical, behavior, or cognitive) or by geographic location of damage in the brain (frontal, parietal, temporal, occipital, limbic, hypothalamic, etc.).
Some of the most common symptoms of mild TBI are:
- Headache
- Confusion
- Lightheadedness
- Blurred vision
- Tinnitus recovery
- Sensitivity to sound and light
- Nausea and vomiting
- Sleep disruption
- Mood and behavioral changes
- Difficulty concentrating
- Poor memory and attention
With more severe TBI symptoms these symptoms can be permanent. Increased severity of TBI also leads to even more disabling symptoms such as:
- Difficulty speaking
- Trouble understanding words
- Increased aggression
- Loss of self-awareness and control
- Poor visual recognition
- Degraded fine motor coordination
The most severe survivable TBIs often lead to persistent vegetative states or profound disability requiring 24-hour specialized care.
Check Your Risk of TBI Today
A common clinical questionnaire useful for screening patients who may be suffering from TBI is the HELPS-TBI tool.
Take it now for free and see if your symptoms might be related to TBI
What is the traditional approach to treatment?
Treatment for TBI has traditionally been focused on those with significant disabilities. These are usually individuals who required hospitalization for moderate to severe TBI. Their rehabilitation program will be determined by the nature and severity of their injuries, degree of resulting impairment and disability, overall health, and social and family support. There are a variety of brain treatment programs for moderate to severe TBI which include:
- Acute rehabilitation
- Long-term rehabilitation
- Transitional living
- Behavioral management
- Day-treatment
- Independent living
The general domains these programs focus on are physical care, self-care and activities of daily living, mobility skills, communication and cognitive skills, socialization, vocational retraining, counseling, and education.
However, a vast majority of TBI are mild, even those that are evaluated in an acute care setting such as the emergency department and have advanced diagnostic imaging like a CT scan. For those diagnosed with mTBI/concussion there is traditionally very little support and guidance. Usually, you will just get instructions for cognitive rest, encouragement for quality sleep and nutrition, avoiding intoxicants (alcohol), and graduated return to play protocol (if applicable). Anti-inflammatories and anti-nausea medicines are commonly used in the acute phase of injury.
The traditional approach to management of mTBI/concussion does not address the underlying causes of the secondary phase of TBI injury. This traditional approach is fine for many people; however, a substantial portion of people who sustain a mTBI will develop persistent symptoms. Over time, the association between the symptoms and the mTBI is lost, or never made (especially for those who did not enter the health system to being with). Eventually, if medical attention is obtained, treatments are initiated to mitigate the symptoms. Patients can readily find themselves on a potent cocktail of psychostimulants (methylphenidate), antidepressants (fluoxetine, escitalopram), anti-inflammatories (meloxicam, diclofenac), antispasmodics (cyclobenzaprine, tizanidine, baclofen), neuropathics (gabapentin, pregabalin), narcotics (hydrocodone, oxycodone), and benzodiazepines (lorazepam, diazepam) in an honest attempt to make them feel better. Unfortunately, this is typically a self-defeating strategy as the medication interactions and effects frequently lead to feeling more groggy, detached, and depressed. All of these treatments may help mask the effects of the injury, but do not treat the underlying, non-neuropermissive environment created by the secondary phase of injury.
Additional Resources (links to learn more about program)

TBI Help Now – Dr. Mark Gordon’s Website

The Joe Rogan Experience Podcase #1589 – Dr. Mark Gordan & Andrew Mar

The Joe Rogan Experience Podcast #700 – Dr. Mark Gordan & Andrew Marr
Quiet Explosions: Healing the Brain. Winner of the Lilac Award – SPIFF International Film Festival.
Dr. Mark Gordon – A complete Cure for Anxiety, Depression, OCD, Bipolar, PTSD, Addiction?
Dr. Mark Gordon on ESPN: Outside the Lines
Free Thinking with Montel Williams Podcast – Dr. Mark Gordon & Jerri Sherr
How do I get started?
Choose one of Asymmetric Health’s Evaluations to begin. If you’d prefer to talk it through first, schedule a free, no-obligation consultation. We’ll review your symptoms, answer your questions, and walk you through our membership and enrollment process.
Learn More About TBI Evaluation…
Schedule a Free Consultation…
Text Resources
Gordon, Mark L. The Clinical Application of Interventional Endocrinology. Phoenix Books, Inc, 2007.
Gordon, Mark L. Traumatic Brain Injury: A Clinical Approach to Diagnosis and Treatment. 2.0 ed., Millennium Health Centers, Inc., 2016.
Huang, Canhua, and Yuanyuan Zhang, editors. Oxidative Stress: Human Diseases and Medicine. Springer, 2021
“TBI Data.” Traumatic Brain Injury & Concussion, Centers for Disease Control and Prevention, 11 May 2021, https://www.cdc.gov/traumaticbraininjury/data/.